2.10. In connection with Micromovements
2.10.1. Summary
As the movements, according to their nature, have a markedly different consequence on the medium-term behavior of the implant in the bone, I have established a distinction between the movements observable radiologically and macroscopically, and the non-observable relative movements of very small amplitude, which I called Micromovements, which regularly damage the bone-implant interface and prevent secondary stability from being established through Osseointegration.
Micromovements are at the origin of the migration of rigid implants.
The anchoring of the prosthesis must prevent the appearance of small movements in the bone bed likely to damage the bone cells and prevent them from forming their crystalline component in the immediate vicinity of the implant.
The choice of a thin Titanium wall that I made for the Bicon cup allowed the elimination of bone-implant Micromovements, the bone and the Titanium deforming simultaneously, macroscopically and microscopically, and thanks to this the migrations of acetabulum was removed.
2.10.2. Micromovements and Macromovements
It seemed useful to me to make a distinction between on the one hand movements of very low amplitude, not detectable radiologically, but exceeding the order of magnitude of the size of bone cells, which do not necessarily compromise long-term stability, and which I call Micromovements,
and on the other hand the movements of an implant in relation to its bone bed, the effects of which are visible and measurable on an x-ray, due either to the absence of primary stability or to loosening, which are Macromovements.
In order for the secondary fixation of the prosthesis in the bone bed to be established during the weeks or months following implantation, the immobilization must reach a level of quality compatible with Osseointegration as described by the Professor Felix Lintner.
The surface microstructure of titanium prostheses, obtained by projection of corundum grains (variety of aluminum oxide crystals), includes craters of the same order of magnitude as bone cells as well as finer structures.
The surface microstructure, obtained by plasma spraying of biomaterials such as hydroxyapatite, presents crevices of the same order of magnitude. Thanks to this, the surface thus created is significantly larger than a smooth, polished surface.
2.10.3. Consequences of relative movements between implant and bone
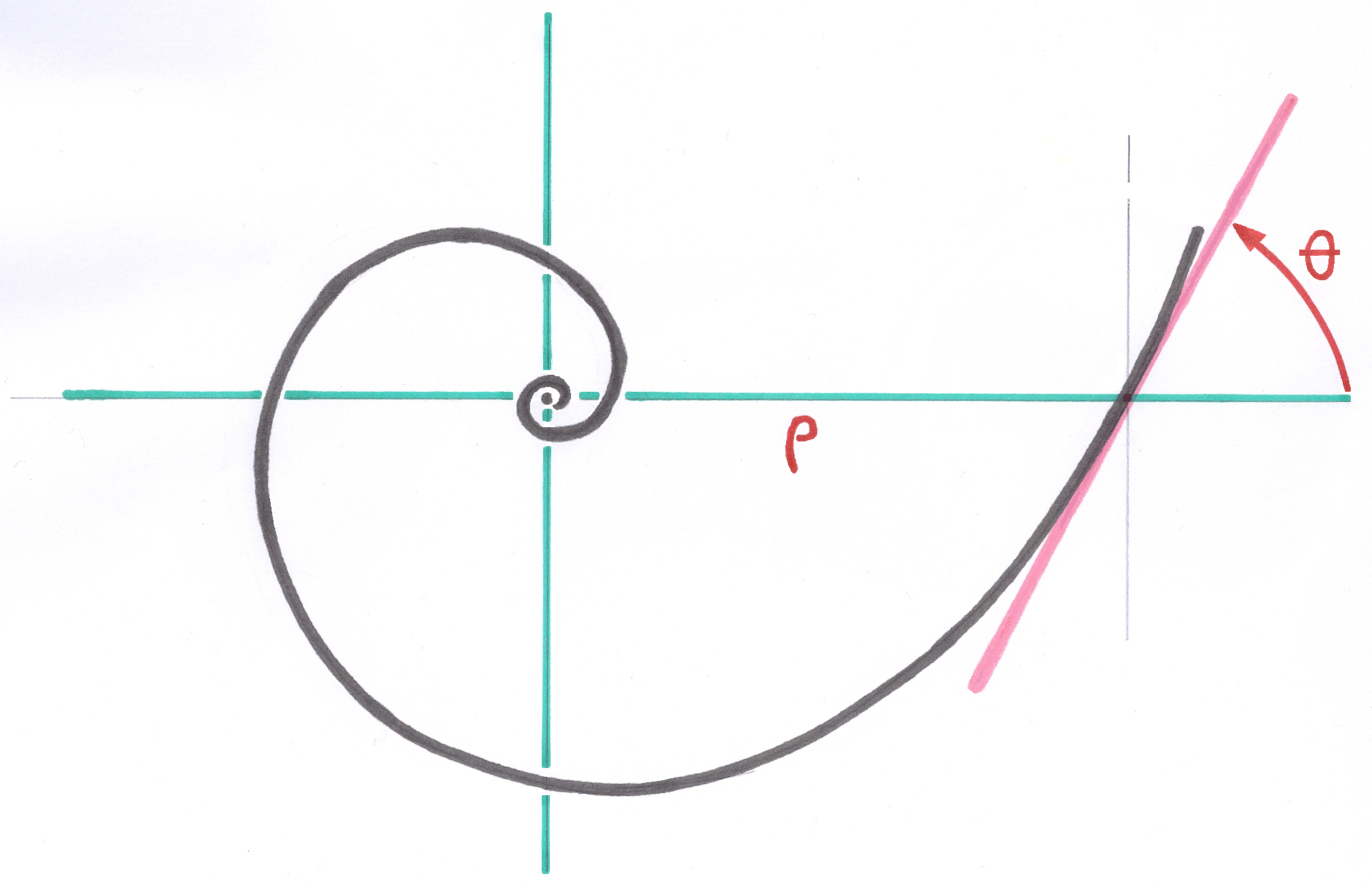
Consider a specific point of a bone-implant assembly in contact and at rest.
If a bone cell with a dimension of the order of 30 microns facing a crater in the metal were regularly subjected to translations (slidings) of 100 microns in the macroscopic plane of the junction, these translations would have the effect, at least, of prevent this bone cell from building up its local crystal structure and at worst destroying this bone cell, similar to a rasp, even if this happens occasionally. All that remains in this zone of the interface is soft and amorphous connective tissue, with no crystalline component. Osseointegration does not take place.
If, on the other hand, the translational movements remain below the size of the cells, the bone cell is not damaged and can build its crystalline structure. If in addition, periods of rest and absence of intensive movements allow a specific point of the assembly to be neither stressed nor damaged, then I consider that there is no longer any obstacle of order mechanical or geometric to osseointegration.
Even when the mechanical situation allows sufficient immobilization and suppresses micromovements, this is still not enough to achieve osseointegration, because the stimulation of bone regrowth and the conditions of biocompatibility must also be satisfied.
2.10.4. The need for preconstraint
It is the Preconstraint provided by the Geometric Anchoring which makes it possible to eliminate the micro-movements that would occur if the prosthesis had the possibility of deviating from its bone bed and then of approaching it at the occasion of alternating solicitations. The role of the Preconstraint is to permanently exert sufficient force to compress the prosthesis against the bone, a force which must always be greater than that tending to separate the prosthesis from the bone. When osseointegration is achieved and the tensions to which the bone was subjected after implantation have disappeared, the Preconstraint no longer has the usefulness it had during the stage when only primary stability allowed the functioning of the prosthesis. .
The absence of micromovements at a specific point does not mean the total absence of macroscopic deformation. If the implant and its bone environment deform simultaneously with very similar amplitudes during successive loadings, including occasionally heavy loads, micromovements do not necessarily appear. If the micromovements are eliminated, the bone and the implant remain locally in intimate contact over large areas. The bone-prosthesis assembly behaves as if it were a one-piece object made up of a single, continuous material.
2.10.5. About isoelasticity
I will call this ideal if not utopian situation, which we seek to achieve thanks to the Geometric Anchoring by respecting the Distributed Constraints and the Preconstraint, the true isoelasticity.
In my opinion, a hip prosthesis would be isoelastic if, for a patient, the elastic deflections of the center of the prosthetic head were of the same amplitude as those which could have been observed (if the measurement method existed) on the hip before the implantation, or on the contralateral hip, with identical constraints.
About thirty years ago, with a little too much ease and illusion, the expression "isoelastic" was used to describe implants that were flexible, elastic, but whose deformability far exceeded the natural deformation of the 'bone. Today, about these implants, I prefer to talk about hyperelasticity.
The hyperelasticity of these implants allowed millimetric macromovements of the implant in the bone bed causing numerous wear debris. In addition, the use of Polyacetal and Polyethylene directly facing the bone, whose pellicular fragments, of microscopic dimensions but the large number of which creates a large surface, detached by macromovements, destroy the surrounding bone, has led to a high proportion of reoperations.
2.10.6. Movements in the trochanteric area
In a femur having received a hip prosthesis, the trochanteric zone behaves differently. Since the trochanteric zone does not completely surround the femoral stem, it cannot benefit from the same advantages as those brought to the cortical anchoring zone by the Conical Junction.
I don't think that it is always the prosthesis which moves away elastically from the bone of the trochanteric massif but rather that it is the greater trochanter which is subjected, during loading, to strong tractions which tend, by moments, to spread it laterally from the metaphyseal part of the stem.
These macroscopic elastic movements of separation are, in my opinion, at the origin of the observable borders in the region of the trochanteric aileron (zone 1) and I do not believe that a prosthesis designer can improve this situation.
I don't think these edgings always have a negative meaning for the upper. A risk may however come from wear debris resulting from the friction of the head in the acetabulum which may be deposited in the edging.
----
Next: